Summer COPD brings our FLASS patients extra challenges. And so, we want to bring you this Summer Guide for 2019. We hope to help you cope with the summer. symptoms, triggers, and challenges.
Chronic Obstructive Pulmonary Disease. (COPD) causes suffering for you and your loved ones. We hope some of the knowledge, tips and hints in this blog will help minimize the summer misery. Likewise, this blog begins a special journey for you because we are updating and creating a Florida Lung, Asthma and Sleep Specialists Official Summer Guide to COPD. This journey will continue through the next three blogs. If you or a loved one has COPD, you’re not going to want to miss it.
Summer COPD Heats Up in Florida

A Breath of Summer 2019 and a Summer COPD Guide
Summer COPD brings the patient more than the usual discomfort that we all suffer in the heat. In fact, if you have a chronic obstructive pulmonary disease(COPD) extreme heat and humidity can instigate complications. Here are just a few:
- Summer can intensify your COPD symptoms.
- Special Alert: Be aware that you might experience more than the usual amount of shortness of breath. (dyspnea.)
- Likewise, being exposed to the heat and humidity could ignite bronchospasms.
So we urge you to be prepared and to maintain your medications with extra vigilance during these hot months. During the next few blogs, we will be you more bringing tips “to prevent serious summertime complications.”
So, Let us open Part I of the FLASS Summer COPD Guide by going Back to Basics about COPD:
Summer COPD and You: First–Back to the Basics
Assisting Florida Lung Doctor’s Blog is our highly qualified guest expert Nancy Albritton. Nancy is a Registered Nurse in Texas. We welcome the participation and expertise she brings to this blog. She states, “Treatments for Chronic Obstructive Pulmonary Disease, otherwise known as COPD, have come a long way the last 46 years of my nursing career with many good changes.”
And she adds, “Just about everyone has either lost friends and/or loved ones due to this condition. Many have family that are plagued by one of the four stages of COPD.”
- COPD is the 3rd leading cause of death in America.
- There are over 11 million diagnosed cases.
- And there are 24 million more suspected cases. These are the ones that may not even realize they have COPD.
There is a tremendous amount of new information that is pertinent to this disease. First, let’s touch on some of the basics before bringing you specific information on coping with summer COPD.
Starting off with simple things, we’ll define exactly what COPD means, by defining what each letter of this acronym represents.
“C” is for Chronic

Only testing and research can help us better understand the problems of COPD.
Chronic is a medical term to describe a disease that does not go away. Not even when you’re feeling at your best.
Likewise, even if you’re not having any symptoms today, you know they will be back tomorrow. You are still chronic because you deal with the disease and its effect constantly.
“O” Means Obstructive:
The obstructive symptom of COPD indicates you have trouble getting the air out of your lungs. This makes it difficult also to bring fresh air into your lungs. It’s a vicious cycle.
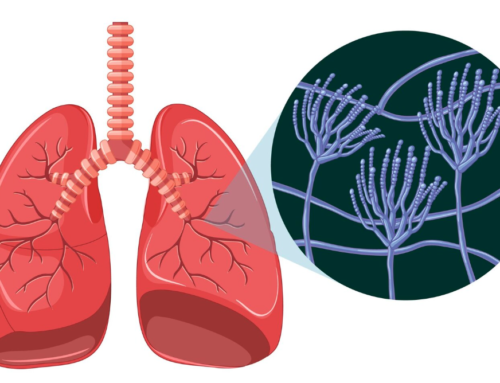
“P” Stands for Pulmonary:
Any time you hear a sickness described as “Pulmonary,” realize that by definition it means “a disease of the lungs.”
“D” Signifies Disease:
Although we take the term “disease” for granted in a mainstream language, it is also a medical term. The D for Disease in COPD explains that it is a medical condition with symptoms that affect structure or function or both.
Introducing the COPD Staging System: What Stage are You?
COPD is not an all-or-nothing condition. It has levels of severity. In 2011, the Global Initiative for Obstructive Lung Disease (GOLD) devised a staging system to help physicians develop appropriate treatment plans. There are four total stages of COPD:
Stage I: Mild COPD:
In Stage I, you or your loved one notices the airflow is somewhat limited. But you don’t notice it much. Of course, sometimes you think it is just “getting older,” or “just my imagination.” You notice that you have a cough and you bring up mucus every once in a while. According to the Mayo Clinic, during the early stages of COPD, most people require little or no medication. Typically using a short-acting bronchodilator, such as albuterol, is all that’s required. The medication relaxes the muscles in the walls of your airways. This can help relieve coughing and shortness of breath and make breathing easier
Stage II: Moderate COPD
Your airflow is decidedly worse, with almost daily involvement. You’re often short of breath, and especially so after doing something active. This is the point where most people notice symptoms. Then, they realize they must get help coping with the condition. At level II, the disease has begun to interfere with your normal life activities.
In the early stages of COPD, most people require little or no medication. “Typically using a short-acting bronchodilator, such as albuterol, is all that’s required. The medication relaxes the muscles in the walls of your airways. This can help relieve coughing and shortness of breath and make breathing easier. If symptoms continue despite albuterol, a long-acting bronchodilator, such as tiotropium or salmeterol, may be helpful.”
Stage III: Severe COPD
Your airflow and shortness of breath are worse. You discover you can’t do normal exercises anymore. Your symptoms flare up frequently. This “flare UP” is also called an exacerbation.At this time, you may discover that minor illnesses like the flu hits you harder. You may feel that you need to rest more frequently after minor exertion. In some cases, you may not maintain a full schedule at work. At this point exacerbations will hit you harder and last longer.
Stage IV: Very severe COPD
During this stage IV , your airflow is limited. Also, your flare-ups are more regular and intense and your quality of life is poor. Just as individual people differ, symptoms of COPD can be different for each individual. However, below are some fairly common symptoms from Stage 4 of COPD, whether it is summer,fall or winter.
- Increased shortness of breath.
- Frequent coughing with and without mucus.
- Increased breathlessness.
- Wheezing.
- And tightness in the chest.
Severe COPD definitely requires treatment. And there are many other factors to consider relating to treatments. Through tests or consultation, your pulmonologist or healthcare provider will determine how your individual symptoms will affect you every day.
Likewise, your physician will then be able to devise an action plan for treatment. And be aware that the medications and treatments will change over time with the progression of your COPD.

During a COPD Summer, Never Forget Your Rescue Medicine
Summer COPD: Co-Existing With Your Other Health Issues
Your pulmonologist will view the COPD within the framework of your entire health profile. Potential health problems such as high blood pressure, heart disease, heartburn, depression, diabetes are factors to consider. These medical problems can determine how COPD affects you and how you and your doctor can manage it.
There are other things to consider besides the numbers in monitored breathing tests (spirometry) or lung function tests. Your doctor may order tests to determine your level of care. We must answer two important questions prior to outlining care. Or as we like to call it, outlining Your COPD Action Plan:
- Number One: Did you have a cough? Do you cough up mucus most days for at least three months in a period of at least two years? (If yes, you may have a chronic bronchitis type of COPD. This type will respond to different medicines)
- Number Two: Are your lungs stretched out and larger than normal? If this is the problem, then you may have an emphysema type of COPD. (Sometimes the size of the lung can be decreased so it will work more effectively, but that is a story for another blog.
Recent Research and Testing
Registered Nurse, Nancy Albritton reminds us that an estimated $1.5 billion yearly is spent just for COPD admissions. Nobody wants to keep returning for COPD hospital readmissions. (or any other reason for that matter).
In my home state of Texas (Dallas area), a study was started in 11/2016 with 267 COPD patients. This study was aimed at hopefully reducing the facility readmissions rate. The rate at the start of their study was 21.3% COPD readmissions. This figure was reduced to 16.2% by the completion of the study.
So how did they so significantly lower this readmissions rate for their COPD patients? As it turns out, the Dallas Area Study lowered that readmission rate in much the same way that we at FLASS have lowered ours: Teamwork and patient communication.
Their key recommendation was to form a coordinated effort of individuals from different disciplines. And importantly, They are medical people that are passionate and knowledgeable about the patient’s respiratory care. This key is also central to the success at FLASS, where testing and research has confirmed the value of a caring team approach with COPD patients.
Commitment to your health journey comes from every level of care.
- the pulmonologist,
- the Respiratory Therapist,
- the Physical Therapist,
- and dietitian.
As you know from previous blogs, FLASS likewise places maximum focus on Patient-Centered values.
Summer COPD and Our Patient-Centered Approach
As is true in many life situations, FLASS knows that patients tend to perform better when they love what they are doing. In this way, better results for all are achieved.
That is why Florida Lung, Asthma and Sleep Specialists strive at every level to improve your quality of life. It’s also why we say that when you are here, you are family. In fact, even when you are not here, you can maintain constant communication with your FLASS healthcare team through our FLASS connect system.
Our Terrific Tip Number One

It Takes a Team to Control Summer COPD
or Summer COPD 2019 Part I
During the hot summer months, you should increase your fluid intake regardless of your activity level or thirst.
- Did you know that Water loss from the body (through sweating) can range from 0.3 liters/hour up to 6.0 liters per hour?
- The combo of heat and activity can cause you to become quickly dehydrated and go into exacerbation of your COPD. Just, remember to compensate for water loss with fluid intake. Thank you for reading our blog at FLASS and remember that we’ll be spotlighting Summer COPD 2019, in our next 3 blogs.